By Miranda So, Jenny Curran, Shahid Husain, Qian Li, Mark McIntyre
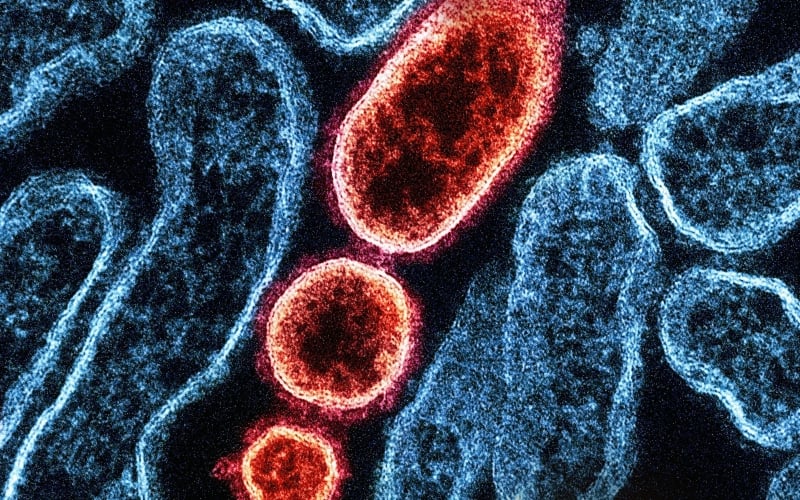
Antimicrobial resistance (AMR) long has been described as a “slow-moving tsunami,” giving the impression that while it is indeed something apocalyptic, the fallout is only going to be felt in the vague, distant future. It may seem that we do not need to take immediate action because there is still time … but is there?
Unfortunately, time is not on our side. In the backdrop of the COVID-19 pandemic, AMR, which predates COVID-19, is becoming more widespread. The fallout of AMR is felt in the present, not the future. It has the potential to affect a wide swath of the population rather than only the most severely ill. In Canada, in addition to having limited access to new antimicrobials, ongoing supply chain challenges with existing antimicrobials (for example, the current shortage of amoxicillin) also affect our ability to treat infections. In short, AMR is a global public health threat.
Antimicrobial use – antibacterials, antifungals and antivirals – has led to the emergence of AMR. The pandemic has exacerbated the situation.
Early in the pandemic, the assumption that patients with COVID-19 had a high likelihood of bacterial co-infections led to a disproportionately high prevalence of antibiotic prescribing relative to the actual prevalence of bacterial co-infections. A meta-analysis of 154 studies conducted between December 2019 and May 2020 found that three out of four patients hospitalized with COVID-19 received antibiotics, yet fewer than one in 10 had bacterial co-infections that warranted therapy.
As the pandemic evolved, evidence-supported therapies against COVID-19 became better standardized, and supportive care such as mechanical ventilation and extracorporeal membrane oxygenation (ECMO), offered life-saving benefits. However, with prolonged hospitalizations, patients are at risk of acquiring infections associated with health care as well as secondary infections that could drive the need for antimicrobial use.
Repeated exposure to antibiotics can result in the emergence of multidrug-resistant bacterial infections and invasive fungal infections, both of which are significant complications and can cause death. Considering the volume of patients who were hospitalized during the successive waves of COVID-19 locally, nationally and globally, we have seen a lot of antimicrobials being prescribed, contributing to a rise in AMR.
Globally, antibiotic resistance has increased since COVID-19 began.
Trying to save the life of a patient fighting an infection caused by extremely antibiotic-resistant bacteria is more common than one would think. It is a devastating situation for patients, their loved ones and the health-care team. To make matters worse, the impact of antibiotic resistance goes beyond the patient who received antibiotics, with implications on the resistance patterns at the ward and facility level. Globally, antibiotic resistance has increased since COVID-19 began. Since we live in a connected world, as the spread of SARS-CoV-2 has taught us, antimicrobial-resistant pathogens can spread globally and quickly. Put another way, what is happening in seemingly faraway places is already affecting us directly.
“The thoughtless person playing with penicillin treatment is morally responsible for the death of the man who succumbs to infection with the penicillin-resistant organism.”
– Sir Alexander Fleming, Nobel Laureate
Antimicrobial resistance affects you, me – everybody
Without effective antimicrobials, the medical advances of the past few decades – many of which are life-saving miracles, and many of which we now take for granted – are at peril: a cut on the skin can cause an infection, causing someone to lose their limb or their life without effective antibiotics.
Anyone undergoing routine procedures such as C-section, hip or knee replacement face an unacceptable risk of post-surgical infections without effective antibiotics, which can lead to long term disability, poor quality of life, and even death from C-section complications. With our aging population, the number of Canadians needing hip or knee replacements will continue to increase in the next few decades. That is a huge swath of the population whose mobility may be taken away as a consequence of AMR.
Cancer treatment has advanced in leaps and bounds and more patients are being offered life-prolonging therapy than before. But cancer treatment increases one’s vulnerability to infections. Therefore, treatment cannot proceed without the support of effective antimicrobials; the last thing we want to see is patients surviving cancer only to succumb to an untreatable infection.
Solid organ transplantation gives patients a new lease on life. However, without effective antimicrobials, the surgery of transplantation cannot take place due to unacceptable risks of infections. Even if someone survives the surgery, it is not feasible to sustain the life-long immunosuppression required to prevent rejection of the transplant without effective antimicrobials.
All of us can take an active role in tackling AMR
Whether we are healthy individuals, patients, health-care professionals, health-care leaders or policy-makers, we all have a role to play to slow down the onslaught of AMR. Sir Alexander Fleming, who discovered penicillin and changed the course of human history, predicted the emergence of antibiotic resistance and its devastating effect on human life shortly after winning the Nobel Prize in 1945.
We all need to understand why antimicrobials are not necessarily the answer to all infections, and tackling AMR goes beyond optimizing antimicrobial use. Immunization against pneumococcal disease, for example, is highly effective at reducing the risk of infection, thereby reducing the need for antibiotic treatment. The annual flu shot reduces the risk of the flu, thereby reducing the risk of secondary bacterial infections following influenza and subsequent need for antibiotic treatment.
Although antimicrobial stewardship programs have been established in many acute-care hospitals and complex continuing-care facilities, they receive limited resources. Furthermore, outpatient antimicrobial stewardship remains under-developed in Canada. Given the bulk of antimicrobials are prescribed in outpatient settings, especially in walk-in clinics where many Canadians rely on for health-care access due to national shortage of family physicians, dedicated resources such as the Four Moments of Antibiotic Decision-Making from the U.S. AHRQ and the outpatient toolkit from Public Health Ontario are helpful to primary-care clinicians. A vital aspect of the outpatient interventions is to empower patients to better understand the benefits and harms of antimicrobial use, which remains an unmet need.
For policy-makers, a timely, robust surveillance system of antimicrobial resistance, coupled with efficient tracking of antimicrobial consumption will help direct antimicrobial stewardship efforts in a coordinated fashion across Canada and at the global stage.
Antimicrobial resistance is not a slow-moving tsunami. Rather, it is a public health threat that is fast and furious. Everyone has a role to play to mitigate against this threat, and we must act now. Nov. 18-24 is World Antimicrobial Awareness Week – let’s spread awareness, not resistance.
![]()
—
This post was previously published on HEALTHYDEBATE.CA and is republished under a Creative Commons license.
***
You Might Also Like These From The Good Men Project
 Compliments Men Want to Hear More Often
Compliments Men Want to Hear More Often  Relationships Aren’t Easy, But They’re Worth It
Relationships Aren’t Easy, But They’re Worth It  The One Thing Men Want More Than Sex
The One Thing Men Want More Than Sex  ..A Man’s Kiss Tells You Everything
..A Man’s Kiss Tells You Everything Join The Good Men Project as a Premium Member today.
All Premium Members get to view The Good Men Project with NO ADS.
A $50 annual membership gives you an all access pass. You can be a part of every call, group, class and community.
A $25 annual membership gives you access to one class, one Social Interest group and our online communities.
A $12 annual membership gives you access to our Friday calls with the publisher, our online community.
Register New Account
Log in if you wish to renew an existing subscription.
Username
First Name
Last Name
Password
Password Again
Choose your subscription level
- Yearly - $50.00 - 1 Year
- Monthly - $6.99 - 1 Month
Credit / Debit Card PayPal Choose Your Payment Method
Auto Renew
Subscribe to The Good Men Project Daily Newsletter By completing this registration form, you are also agreeing to our Terms of Service which can be found here.Need more info? A complete list of benefits is here.
—
Photo credit: iStock.com
The post Antimicrobial Resistance: ‘Slow-moving Tsunami’ Now Coming Fast and Furious appeared first on The Good Men Project.
Original Article